Clinically reviewed by Chris Mosunic, PhD, RD, MBA, Chief Clinical Officer, Calm
Healthcare leaders are in a bind when it comes to driving growth for their organizations, a top priority for nearly two-thirds of them. Despite tight margins and severe workforce shortages, they must find ways to improve the patient experience, attract new customers, and grow revenue.
More than half of healthcare executives (53%) aim to do this by increasing productivity and cost efficiencies. Nearly half of leaders (46%) will try to rebuild consumer trust by keeping the cost of care in check.
To drive these goals forward, leaders are implementing a variety of strategies, including investing in digital technologies for patient virtual visits, remote monitoring, and communication; upskilling clinicians to the top of their license; introducing new health and wellness products, particularly to address health inequity; and strengthening cybersecurity to protect patients and the organization.
But perhaps one of the most critical growth strategies healthcare leaders can pursue is investing in the mental health and well-being of its professionals. Nearly 60% of healthcare organizations expect continued workforce shortages and other challenges. Supporting the mental and emotional well-being of nurses, doctors, and other clinicians can help healthcare organizations improve retention, productivity, and the patient experience while also helping them control escalating healthcare claims costs.
The hidden cost of unmanaged mental health in the workforce
Indeed, chronic stress—pervasive among nurses and physicians—affects the body and behavior in myriad ways that can escalate healthcare utilization and result in higher healthcare claims costs for their employers.
For instance, healthcare workers with chronic stress may suffer from a variety of concerns such as fatigue, lack of focus, nausea, headaches, or muscle pain. They might begin to overeat, scale back on exercise and socializing, or increase their use of alcohol or tobacco. Left unaddressed, chronic stress may ultimately lead to serious mental and physical health challenges, from anxiety and depression to diabetes, stroke, and heart disease.
These conditions, especially when untreated, can significantly escalate employers’ healthcare costs. Twenty of 29 studies reviewed by the US Government Accountability Office showed that higher healthcare costs are associated with adults with untreated behavioral health conditions. One survey analysis showed that people with unrecognized depression incur 149% higher direct healthcare costs than those without symptoms of depression and 38% higher than those with recognized depression.
Of course, workforce mental health challenges also lead to significant indirect costs. Workers with fair or poor mental health are estimated to have nearly 12 days of unplanned absences per year compared to 2.5 for other workers. The cost of a missed workday is estimated to be $340 per day for full-time workers.
Similarly, a large-scale depression costs study found that indirect costs exceeded direct costs. For every dollar spent on depression-related direct costs—medical services and medications—an additional $2.30 was spent on depression-related indirect costs—missed work days and reduced productivity at work.
Proactive mental health support is important to help control costs
Clearly, healthcare organizations aiming to improve productivity and profitability should consider mental health support that helps people with stress, mild symptoms of depression and anxiety, insomnia, and other concerns before they become significant health problems. According to an analysis by consulting firm McKinsey, only 24% of employees require counseling and 1% require a mental health prescription medication. By contrast, 75% of employees need support that promotes mental well-being.
But the challenge for healthcare organizations is offering mental health support that their staff will actually use. A wide range of barriers must be overcome, from stigma and fear of judgment or loss of a medical license to a lack of awareness and busy schedules. For example, one study showed that 50% of frontline healthcare workers didn’t know how to access their employee assistance program (EAP).
Digital mental health apps such as Calm Health remove many of these friction points by offering instant, stigma-free access to programs for stress, mild depressive symptoms, anxiousness, insomnia and other challenges.
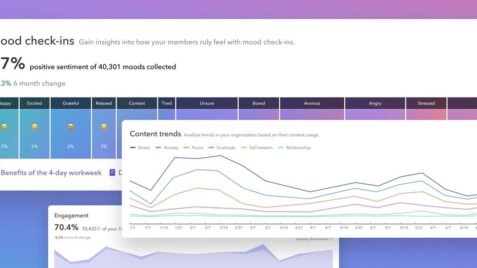
Additionally, Calm Health guides users to appropriate mental health support by tailoring recommendations to their screening results, personal goals, and self-reported conditions and topics of interest. These resources include not just Calm Health evidence-based programs and mindfulness content, but also an organization’s EAP and other resources, helping boost awareness and utilization across the workforce.
How workforce mental health can improve the patient experience
The mental well-being of doctors, nurses, and other healthcare professionals doesn’t just help control costs; it’s critical to the patient experience, positive patient outcomes, and the reputation of the healthcare organization.
For example, research from the American Hospital Association and Press Ganey has shown a direct link between the well-being of the healthcare workforce and the patient experience and safety outcomes in hospitals. The data shows that care gets safer as the experience and well-being of the workforce and patients improve.
Further, the most impactful driver of the patient’s reported experience of care is the teamwork of care team members, according to the study. High scores on team member engagement surveys go hand-in-hand with high patient experience scores and patient likelihood to recommend.
In this way, workforce well-being may have a direct positive impact on a healthcare organization’s quality ratings. Patient experience and the timeliness and effectiveness of care make up about one-third of the Overall Hospital Quality Star Rating, for example. Likewise, the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey of patient perspectives of hospital care is influenced by communication with doctors and nurses and the responsiveness of hospital staff, among other factors.
By contrast, when healthcare workers are chronically stressed or burned out, they’re more likely to struggle with decision making, communicate less effectively, and make more errors, which can negatively affect patient satisfaction scores. Indeed, nurse burnout has been associated with a climate of lower patient safety, more medication errors and adverse events, lower quality of care, and lower patient safety ratings.
A new, evidence-based approach to supporting the mental health of frontline caregivers and other underserved populations
Learn more
Proactive investment pays off, even when budgets are tight
Low morale, low confidence in leadership, and high turnover are additional consequences of clinician stress and burnout, further jeopardizing care quality, the patient experience, and health outcomes. A cross-sectional survey study found that physicians and nurses believe the most important actions management can take are improving nurse staffing and allowing all clinicians to take breaks without interruption.
But offering proactive evidence-based mental health programs is another strategic imperative to support clinicians, patients, and organizations, especially amid tight budgets. In fact, every $1 invested in evidence-based mental health early intervention can yield $2 to $4 in saved costs and better functioning employees.
Calm Health offers evidence-based support for nurses and doctors
A digital mental health platform, Calm Health can play an important role in a health organization’s workforce mental well-being strategy and larger growth goals.
Calm Health offers evidence-based programs developed by psychologists and tailored for people with specific health experiences, life experiences, and occupations, including healthcare.
For example, Stress Management for Busy Nurses is a Calm Health series designed to help nurses understand the causes of burnout and support them as they learn to manage symptoms before it becomes habitual. The Physician Burnout: Protecting Your Well-Being series is designed to help physicians avoid burnout by offering practical guidance for managing the unique stressors and challenges they face on the frontlines of healthcare. Both programs are developed by psychologists who are subject matter experts in stress and burnout among healthcare professionals.
Nurses and physicians can also easily incorporate Calm Health’s mindfulness programs into their hectic workdays, even during micro breaks, to relax, find balance, and build resilience. In these ways, Calm Health is not just a wellbeing benefit but a lever for advancing an organization’s broader goals for growth. It’s a proactive strategy that can help leaders create a psychologically healthy work environment, which is associated with reductions in turnover, fewer medical errors, patient safety and health, and a better patient experience.